In recent years, the term ‘leaky gut’ has gained popularity and been proposed as the underlying cause for many medical conditions, including irritable bowel syndrome (IBS). But what does having a ‘leaky gut’ really mean? And does it actually play any role in the underlying cause of IBS?
In scientific terms, ‘leaky gut’ really refers to intestinal barrier dysfunction. This describes a state where the gut (or intestine) becomes more permeable (leaky) than usual, potentially allowing bacteria or harmful substances to enter the body when they would normally be kept out.(1, 2)
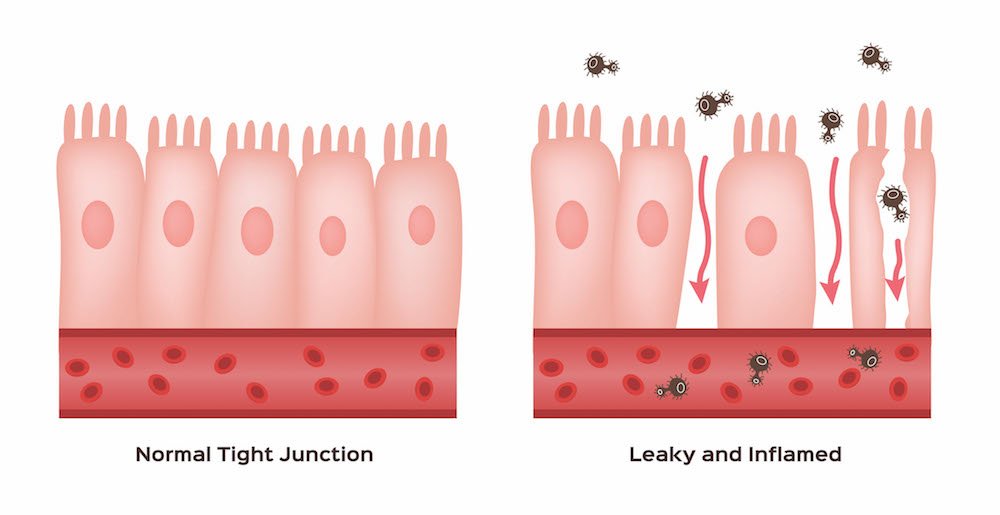
Under normal, healthy circumstances, the cells lining the gut are held together tightly by something called ‘tight junctions’ (see image above), preventing most things that are foreign or nasty from crossing through the gut and into our body where they could cause inflammation or infection.(1, 2) This is why the gut forms such an important part of our body’s immune system, as it acts as a physical barrier and first line of defence from disease causing organisms like bacteria or viruses.(1, 2)
Intestinal barrier dysfunction is known to occur in certain diseases, such as in inflammatory bowel diseases (Crohn’s disease and ulcerative colitis), coeliac disease and intestinal infections (think food poisoning).(3, 4) This is because these diseases or infections involve inflammation, which damages the cells that form the gut barrier. Gut ‘leakiness’ can be treated in these conditions using medications to control the underlying inflammation or infection (or a strict gluten free diet in the case of coeliac disease).(3, 4)
Alcohol and certain medications (especially non-steroidal anti-inflammatory drugs (NSAIDs) like aspirin and ibuprofen) are also gut irritants that can affect the tight junctions between cells in the gut barrier, making them more ‘leaky’.(5) This usually causes little harm or symptoms if use is short term or infrequent, however prolonged exposure can lead to inflammation of the bowel and development of ulcers.(5)
Whether or not changes in gut barrier function are part of the cause of IBS continues to be debated.(1, 2) Of the small number of studies looking at intestinal barrier dysfunction in IBS patients, most have focused on those with diarrhoea predominant symptoms. Some studies have found increased permeability or ‘leakiness’ in both the small and large intestines of IBS patients compared to healthy people, however others have found no significant differences.(1, 2)
Part of the challenge for researchers is that current methods of measuring or diagnosing intestinal barrier dysfunction are suboptimal and more reliable tests need to be developed.(6)
IBS patients have no obvious signs of inflammation when their gut is examined under a microscope, so the clinical significance of ‘leakiness’ or defects in the gut barrier needs to be addressed by future research.(1, 2)
The short answer, no, not that we know of. As mentioned above, it is not definitive that this is indeed a problem for people with IBS and more research is needed to understand this better.
Having said that, a quick Google search of ‘how to fix a leaky gut’ suggests that there are all kinds of treatments, gut health supplements and special diets available to correct this problem. However, it should be noted that there is currently little scientific evidence to support any of these approaches.(1, 2)
One recent study in mice found that feeding of a high FODMAP diet for 2 weeks resulted in an increase in gut permeability when compared to mice fed a standard diet.(7) The same study also showed that a 4-week low FODMAP diet could normalise intestinal permeability in rodents subject to high levels of stress (psychological stress is known to increase gut permeability).(7) Whether or not these results actually translate to the human gut is not known, but this is an interesting finding that might shed more light on how a low FODMAP diet provides symptom relief in IBS.
· Current tests used by researchers to identify ‘leaky gut’ have significant limitations and further research is needed to develop more reliable methods
· Whether or not intestinal barrier dysfunction (i.e. leaky gut) plays a key role in IBS is still unknown and the subject of ongoing research
· Avoiding regular exposure to excessive amounts of alcohol and NSAIDs (unless under instruction of a medical professional) may be useful for reducing gut irritation if you have IBS
· There are currently no treatments for ‘leaky gut’ (such as supplements or special diets) that are supported by strong scientific evidence
· A low FODMAP diet might have effects on normalising intestinal barrier function in animal models under conditions of psychological stress, however this is yet to be shown in humans. Regardless, a FODMAP diet approach provides symptom relief for ~75% of people with IBS, so is considered a very effective management strategy for IBS.
References:
1. Martinez C, Gonzalez-Castro A, Vicario M, Santos J. Cellular and molecular basis of intestinal barrier dysfunction in the irritable bowel syndrome. Gut and liver. 2012;6(3):305-15.
2. Matricon J, Meleine M, Gelot A, Piche T, Dapoigny M, Muller E, et al. Review article: Associations between immune activation, intestinal permeability and the irritable bowel syndrome. Alimentary pharmacology & therapeutics. 2012;36(11-12):1009-31.
3. Heyman M, Abed J, Lebreton C, Cerf-Bensussan N. Intestinal permeability in coeliac disease: insight into mechanisms and relevance to pathogenesis. Gut. 2012;61(9):1355-64.
4. Michielan A, #x, Inc, #xe0, R. Intestinal Permeability in Inflammatory Bowel Disease: Pathogenesis, Clinical Evaluation, and Therapy of Leaky Gut. Mediators of Inflammation. 2015;2015:10.
5. Utzeri E, Usai P. Role of non-steroidal anti-inflammatory drugs on intestinal permeability and nonalcoholic fatty liver disease. World journal of gastroenterology. 2017;23(22):3954-63.
6. Galipeau HJ, Verdu EF. The complex task of measuring intestinal permeability in basic and clinical science. Neurogastroenterology & Motility. 2016;28(7):957-65.
7. Zhou SY, Gillilland M, 3rd, Wu X, Leelasinjaroen P, Zhang G, Zhou H, et al. FODMAP diet modulates visceral nociception by lipopolysaccharide-mediated intestinal inflammation and barrier dysfunction. The Journal of clinical investigation. 2018;128(1):267-80.