
Our recently-published review [1] looks at a different approach to how dietary fibres can be used to benefit individuals with IBS. A high-level summary is presented here.
Broadly, ‘dietary fibre’ is an umbrella term that describes any type of indigestible carbohydrate.
There are many different types of fibre, each with distinct physical and chemical properties (e.g., cellulose vs psyllium; Figure 1 below) which dictates their actions along the gastrointestinal tract. These actions (or functional characteristics), in turn, induce specific, physiological responses such as promoting regularity, improving satiety and producing gases via fermentation.
A better understanding of the functional characteristics of different fibres will, therefore, allow us to work out their therapeutic value in IBS, possibly enabling personalised fibre therapy to achieve specific therapeutic responses in patients.

The main functional characteristics of fibre along the gastrointestinal tract are
1. Bulking, which describes how a fibre contributes to regularity, via:
2. Viscosity, which describes whether a fibre thickens when mixed with water and forms gels.
There are many ways of looking at fermentability - the angle of most relevance in IBS is the rate of fermentation:
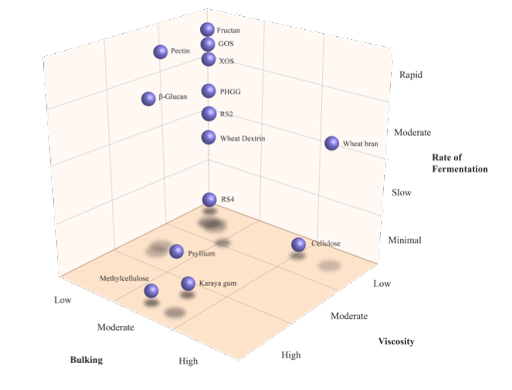
Overview of dietary fibres and their overlapping functional characteristics. Abbreviations: GOS, galacto-oligosaccharides; PHGG, partially hydrolysed guar gum; RS, resistant starch; XOS, xylo-oligosaccharides.
Current clinical guidelines for fibre supplementation in IBS looks at fibres through the perspective of solubility: ‘soluble’ fibres are recommended for reducing symptoms whereas ‘insoluble’ fibres are recommended to be avoided [2, 3]. Issues with such advice are as follows:
This is not an overt criticism of these guidelines given much of the research of fibres in IBS are based on the principle of ‘solubility’ with a ‘one-size-fits-all’ approach and that these recommendations are just a synthesis of what’s available.
We hope that highlighting these functional characteristics will show the number of different ways that fibres can impact our guts and shift the perspective of fibre research in IBS so that specific types of fibre can be investigated and then applied for to achieve specific therapeutic responses, eventually allowing for personalisation of fibres in IBS.