
Following a low FODMAP diet is a well-established approach for managing IBS, with strong evidence showing improvements in both symptom control and quality of life (QoL). More importantly, research has consistently shown that patients achieve the best outcomes when the diet is introduced and tailored by specialist dietitians. Whilst studies have demonstrated that symptom improvements can be maintained for up to 3.5 years, many people with IBS follow this dietary approach for longer. Therefore, understanding the diet’s sustained effects is crucial. Current evidence on the longer-term outcomes of the diet remain limited and inconsistent, especially food-related QoL outcomes. Thus, this study aimed to evaluate the long-term outcomes of patients who received dietitian-led education on the low FODMAP diet for IBS, providing insight for up to seven years after their initial intervention.
A total of 74 IBS-diagnosed patients who consulted a specialist dietitian between 2008 and 2018 were included in this study with these outcomes measured:
Participants were followed for an average length of 7.1 years.
During the initial dietitian-led education process, only 46 (62%) completed the FODMAP reintroduction step and 17 (23%) successfully progressed through the personalisation stage of the diet. Of which, only 7 of them reintroduced tolerated FODMAPs back into their diet.
Nine participants (12%) continued to follow a strict low FODMAP diet, meaning they were stuck in step one. However, 62% (n=46) reported following a personalised diet with at least one FODMAP group restricted and eating patterns that resembled a healthy population. Despite this, two-thirds of the participants were able to satisfactorily control their symptoms even six years after follow-up. Identifying individual FODMAP triggers and avoiding them appeared to be key for long-term symptom relief. Interestingly, the participants who continued to restrict FODMAPs reported lower food-related QoL outcomes compared to those who were consuming a habitual or personalised FODMAP diet.
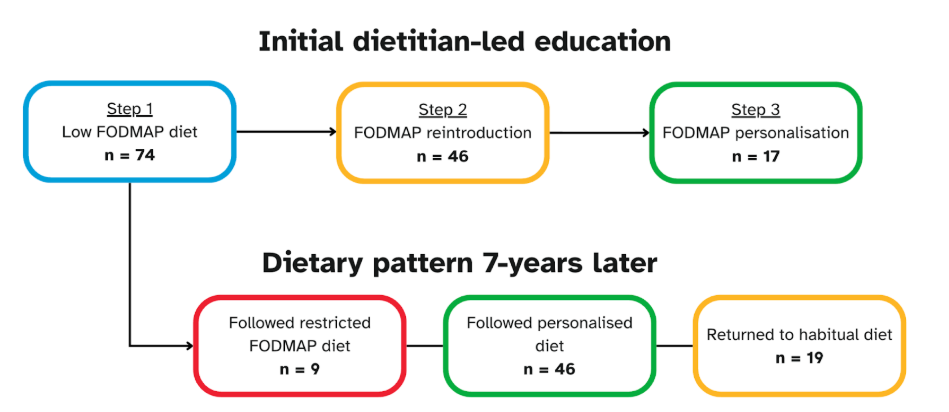
^Figure 1. Flow diagram of the number of participants who completed each step of the FODMAP diet during the initial dietitian-led education process, and their dietary patterns. Participants were followed for an average length of 7.1 years.
Although not all participants completed every stage of the diet, most agreed that guidance from a dietitian was far more valuable than advice from a gastroenterologist or general practitioner. Many felt more confident and better equipped to manage the diet when supported by a dietitian, particularly because they provided up-to-date resources or suggested to them the Monash FODMAP app and website. In contrast, around half of the participants sought information online, raising concerns about the accuracy of the sources and potentially hindering their adherence.
The findings from this study suggest that long-term adherence to a strict low FODMAP diet is not necessary for symptom control. Instead, maintaining a generally healthy diet while limiting only personal FODMAP triggers appears to be sufficient. Importantly, this approach does not compromise gut microbiota, which has been a major concern with prolonged restriction.
The study also proposed the potential benefits of introducing an additional “maintenance phase” to the diet. This would involve ongoing dietitian support, including tailored advice, updates on FODMAP food composition, and encouragement to reintroduce previously excluded high FODMAP foods where possible.
Overall, these findings highlight the essential role of dietitians in supporting people with IBS on the low FODMAP diet. Their involvement is valuable not only during the initial education phase, but also in providing ongoing guidance to monitor progress, prevent unnecessary restriction, and ensure patients move confidently through all three steps of the diet. With continued support, patients are better equipped to make informed food choices that ultimately promote both effective symptom relief and long-term wellbeing.